Background
Allogeneic hematopoietic stem cell transplantation is the most effective treatment that can cure acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS). However, myeloablative conditioning (MAC) regimens cause high non-relapse mortality (NRM). Reduced intensity conditioning (RIC) regimens can reduce NRM but increase relapse incidence (RI) and as a result of it, has the similar overall survival (OS) to the MAC regimen according to the results of published clinical trials. Nevertheless, most of these clinical trials aren't high quality studies and the results of different studies are not consistent. To clarify whether RIC is as effective as MAC but safer than it for AML in CR and MDS we write the systematic review (SR).
Methods
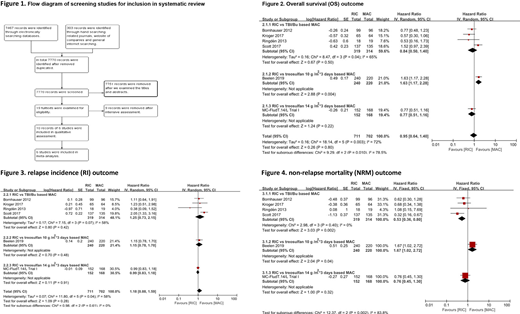
Two reviewers independently comprehensively searched the related databases and websites and hand searched the reference lists. They also independently screened and evaluated the retrieved studies and then extracted data of included studies with the Cochrane Collaboration recommended tools. Only randomized controlled trials (RCTs) were included. Hazard ratio (HR) was used to compare the OS, RI, leakemia free survival (LFS), non-relapse mortality (NRM), the incidence of acute graft versus host disease (aGVHD) and chronic graft versus host disease (cGVHD) with the generic inverse variance method. The III-IV aGVHD and graft failure (GF) were compared with the Mantel-Haenszel method pooled risk ratio (RR). A two-sided P value of less than 0·05 was considered as significant difference. Heterogeneity was significant when the P value of the Chi-square test was less than 0·1 and/or the I2 value was more than 50%. Additionally we used the GRADE principles to evaluate the quality of evidence. The SR was registered on PROSPERO with ID of CRD42020185436.
Results
7770 records were retrieved. We included 6 RCTs with 1413 participants comparing RIC with MAC. Our results showed there wasn't significant difference in OS (HR=0·95 95% confidence interval (CI, 0·64, 1·4), P=0·80) and RI (HR=1·18, CI (0·88, 1·59), P=0·28). Six RCTs and 1413 pariticipants were included of the two outcomes. The result of LFS was (HR=1·09, CI (0·69, 1·74), P=0·71) between RIC and MAC, three studies and 596 participants were included. The heterogeneity was significant in the OS, RI and LFS outcomes so we combined the three outcomes with the random effects model. RIC significantly reduced NRM than TBI/Bu based MAC (HR=0·53, CI (0·36, 0·80), P=0·002), four RCTs and 633 participants were included. On the other hand, RIC didn't reduce NRM than treosulfan based MAC with the results of (HR=1·67, CI (1·02, 2·02), P=0·04) compared with treosulfan 10 g/m2*3 days regimen and (HR=0·76, CI (0·45, 1·3), P=0·32) compared with treosulfan 14 g/m2*3 days regimen, both included only 1 RCT and 460 and 320 participants were included respectively. RIC had a trend to reduce the incidence of aGVHD compared to TBI/Bu based MAC (HR=0·79, CI (0·60, 1·03), P=0·08) and III-IV aGVHD (HR=0·61, CI (0·36, 1·04), P=0·07). RIC didn't show significant difference to treosulfan based MAC regimen on the two outcomes. The heterogeneity of the NRM, aGVHD, III-IV aGVHD was non-significant and we combined the three outcomes with the fixed effect model. The cGVHD was similar between RIC and MAC (HR=1·01, CI (0·79, 1·28), P=0·96), results of included results had significant heterogeneity and random effects model was used. GF was rare in both RIC (2·6%) and MAC (1·1%) arms. The quality of evidence on OS, RI and LFS was moderate and on NRM, aGVHD, cGVHD was high.
Conclusions
For AML in CR and MDS paitents, RIC don't increase OS and RI compared with MAC. RIC regimens reduce NRM than the TBI/Bu based MAC regimens. RIC regimens are also good choice of preparative regimens before HSCT for AML in CR and MDS. The treosulfan based MAC has a promising result in one RCT and even causes less NRM than RIC. Nevertheless, studies are scarce and more studies are needed to confirm the result.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal